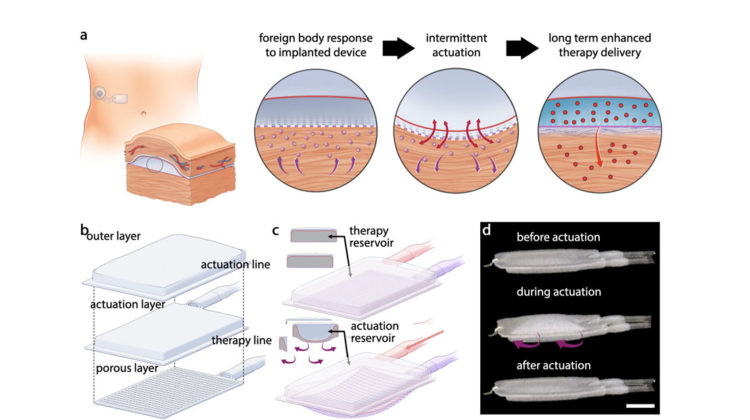
A team of MIT engineers and collaborators has devised a way to prevent the body from building up scar tissue around implantable medical devices, a phenomenon known as the foreign body response.
Implantable devices that release insulin into the body hold promise as an alternative method for treating diabetes without insulin injections or cannula insertions. However, their use has been prevented by the fact that the immune system attacks them after implantation, forming a thick layer of scar tissue that blocks the release of insulin.
However, in a study of mice, the team demonstrated that when they incorporated mechanical actuation into a soft robotic device, the device remained functional for much longer than a typical drug-delivery implant. The researchers found that by repeatedly inflating and deflating for five minutes every 12 hours, the device prevented immune cells from accumulating around it.
‘We’re using this type of motion to extend the lifetime and the efficacy of these implanted reservoirs that can deliver drugs like insulin, and we think this platform can be extended beyond this application,’ said Ellen Roche, the Latham family career development associate professor of mechanical engineering and a member of MIT’s Institute for Medical Engineering and Science.
For many years, scientists have been working on insulin-delivering devices that could be implanted under the skin of patients with diabetes. However, the fibrous capsules that form around such devices can lead to device failure within weeks or months.
In the present study, the researchers built a two-chambered device made of polyurethane, a plastic that has similar elasticity to the extracellular matrix that surrounds tissues. One of the chambers acts as a drug reservoir and the other acts as a soft, inflatable actuator. The device is designed so that insulin can slowly seep out through pores in the drug reservoir or be released in a large burst controlled by the actuator. Using an external controller, the researchers can also stimulate the actuator to inflate and deflate on a specific schedule.
The mechanical actuation drives away immune cells called neutrophils, which initiate the process that leads to scar-tissue formation. When the researchers implanted the devices into mice, they found that it took much longer for scar tissue to develop around them. Scar tissue did eventually form, but its structure was unusual – instead of the tangled collagen fibres that built up around static devices, the fibres that surrounded the actuated devices were more highly aligned, which the researchers believe may help drug molecules to pass through the tissue.
‘In the short term, we see that there are fewer neutrophils surrounding the device in the tissue, and then long term, we see that there are differences in collagen architecture, which may be related to why we have better drug delivery throughout the eight-week time period,’ said visiting scholar Sophie Wang.
The researchers evaluated the effectiveness of the insulin release by measuring subsequent changes in the mice’s blood glucose levels. They found that in mice with the actuated device, effective insulin delivery was maintained throughout the eight weeks of the study. However, in mice that didn’t receive actuation, delivery efficiency began to wane after only two weeks, and after eight weeks, almost no insulin was able to pass through the fibrous capsule.
The authors also created a human-sized version of the device, measuring 120 millimetres by 80 millimetres, and showed that it could be successfully implanted into the abdomen of a human cadaver. ‘This was a proof of concept to show that there is a minimally invasive surgical technique that could potentially be employed for a larger-scale, human-scale device,’ said Debkalpa Goswami a postdoctoral researcher.
The researchers now plan to adapt the device so that it can be used to deliver stem-cell-derived pancreatic cells that would sense glucose levels and secrete insulin when glucose is too high. Such an implant could eliminate the need for patients to constantly measure their glucose levels and inject insulin. ‘The idea would be that the cells would be resident in the reservoir and would act as an insulin factory,’ Roche said. ‘They would detect the levels of glucose in blood and then release insulin according to what was necessary.’
Other possible applications for the device include delivery of immunotherapy treatment for ovarian cancer and delivery of drugs to the heart to prevent heart failure in patients who have had heart attacks. ‘You can imagine that we can apply this technology to anything that is hindered by a foreign body response or fibrous capsule, and have a long-term effect,’ Roche said. ‘I think any sort of implantable drug-delivery device could benefit.’
The research has been published in Nature Communications.