Inspired by sutures developed thousands of years ago, a team of MIT engineers has designed ‘smart’ sutures that can not only hold tissue in place, but also detect inflammation and release drugs.
The new sutures are derived from animal tissue, similar to the ‘catgut’ sutures first used by the ancient Romans. In a modern twist, the MIT team coated the sutures with hydrogels that can be embedded with sensors, drugs, or even cells that release therapeutic molecules.
‘What we have is a suture that is bioderived and modified with a hydrogel coating capable of being a reservoir for sensors for inflammation, or for drugs such as monoclonal antibodies to treat inflammation, said Giovanni Traverso, an associate professor of mechanical engineering at MIT. ‘Remarkably, the coating also has the capacity to retain cells that are viable for a prolonged period.’
The researchers envision that these sutures could help patients with Crohn’s disease heal after surgery to remove part of the intestine. The sutures could also be adapted for use to heal wounds or surgical incisions elsewhere in the body, the researchers said.
Catgut sutures – which are made from strands of purified collagen from cows, sheep or goats (but not cats) – form strong knots that naturally dissolve within about 90 days. Although synthetic absorbable sutures are also available, catgut is still used in many types of surgery.
Traverso and his colleagues wanted to see if they could build on this type of tissue-derived suture to create a material that would be tough and absorbable, and have advanced functions such as sensing and drug delivery.
Such sutures could be particularly useful for Crohn’s disease patients who need to have a part of the intestine removed due to blockage from excessive scarring or inflammation. This procedure requires resealing the two ends left behind after one section of the intestine is removed. If that seal doesn’t hold tightly, it can lead to leaks that are dangerous for the patient.
To help reduce this risk, the MIT team wanted to design a suture that could not only hold the tissue in place, but also detect inflammation, an early warning sign that the resealed intestines aren’t healing properly.
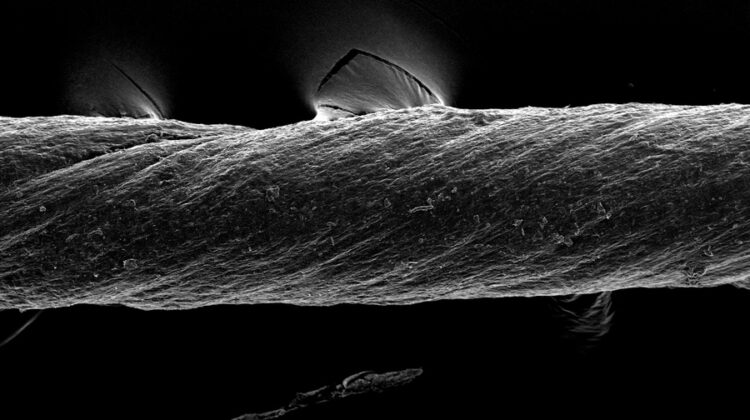
The researchers created their new sutures from pig tissue, which they ‘decellularised’ using detergents in order to reduce the chances of inducing inflammation in the host tissue. This process leaves behind a cell-free material, which the researchers call ‘De-gut’, that contains structural proteins such as collagen, as well as other biomolecules found in the extracellular matrix that surrounds cells.
After dehydrating the tissue and twisting it into strands, the researchers evaluated its tensile strength – a measure of how much stretching it can withstand before breaking – and found that it was comparable to commercially available catgut sutures. They also found that the De-gut sutures induce a much-reduced immune response from surrounding tissue than traditional catgut.
‘Decellularised tissues have been extensively used in regenerative medicine with their superb biofunctionality,’ Lee said. ‘We now suggest a novel platform for performing sensing and delivery using decellularised tissue, which will open up new applications of tissue-derived materials.’
Next, the researchers set out to enhance the suture material with additional functions. To do that, they coated the sutures with a layer of hydrogel. Within the hydrogel, they can embed several types of cargo – microparticles that can sense inflammation, various drug molecules, or living cells.
For the sensor application, the researchers designed microparticles coated with peptides that are released when inflammation-associated enzymes called MMPs are present in the tissue. Those peptides can be detected using a simple urine test.
The researchers also showed that they could use the hydrogel coating to carry drugs that are used to treat inflammatory bowel disease, including a steroid called dexamethasone and a monoclonal antibody called adalimumab. These drugs were carried by microparticles made from FDA-approved polymers such as PLGA and PLA, which are used to control the release rate of drugs. This approach could also be adapted to deliver other kinds of drugs such as antibiotics or chemotherapy drugs, the researchers said.
These smart sutures could also be used to deliver therapeutic cells such as stem cells. To explore that possibility, the researchers embedded the sutures with stem cells engineered to express a fluorescent marker, and found that the cells remained viable for at least seven days when implanted in mice. The cells were also able to produce vascular endothelial growth factor, a growth factor that stimulates blood cell growth.
The researchers are now working on further testing each of these possible applications, and on scaling up the manufacturing process for the sutures. They also hope to explore the possibility of using the sutures in parts of the body other than the gastrointestinal tract.
The research has been published in Matter.